For vaccine manufacturers, the design and validation of an aseptic filling line is not merely an equipment purchase—it is a foundational strategic commitment. The initial design decisions, particularly the choice of barrier technology, irrevocably lock in the facility’s sterility assurance level, operational flexibility, and long-term cost structure. Missteps in this phase can lead to costly revalidation, regulatory delays, and compromised product quality. The pressure to accelerate timelines for pandemic preparedness only amplifies these risks, making a methodical, standards-driven approach non-negotiable.
The regulatory landscape, especially the updated EU GMP Annex 1, explicitly favors advanced barrier systems that minimize human intervention. This shift, coupled with the technical demands of novel vaccine platforms like mRNA, requires a reevaluation of traditional filling line paradigms. Selecting the right system now is critical for ensuring compliance, protecting multi-million dollar batches, and building agile production capacity for future pipeline diversity.
ISO Class 5 Vial Filling Line: Core Design Principles
The Foundation of Sterility Assurance
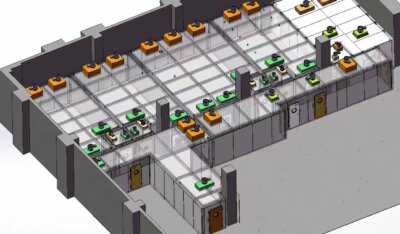
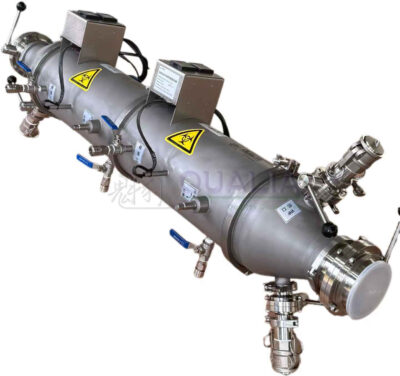
Modern vaccine filling line design is governed by a single imperative: achieving the highest possible sterility assurance level (SAL). This is accomplished by enclosing all critical aseptic operations within advanced barrier systems. The primary engineering control is a positive pressure isolator, which creates a physical separation between the ISO Class 5 aseptic core and the surrounding ISO Class 7 or 8 cleanroom. This isolator provides a unidirectional laminar airflow (LAF) canopy over exposed sterile materials, preventing particulate ingress. A validated automated decontamination cycle, typically using Vaporized Hydrogen Peroxide (VHP), achieves a defined log reduction of biological indicators before each batch. This technological shift from open cleanroom operations or Restricted Access Barrier Systems (RABS) is a strategic imperative for new facilities, as it drastically reduces contamination risk from personnel.
Engineering for Precision and Flow
Beyond the barrier, the line integrates precision mechanisms tailored to product characteristics. For shear-sensitive biologics like mRNA or viral vectors, peristaltic pumps with single-use fluid paths are essential. For more traditional vaccines, highly accurate rotary piston pumps may be suitable. Seamless, sterile material transfer into the isolator is achieved via rapid transfer ports (RTPs) or sterilizable transfer systems. In my experience, the most overlooked detail is the project’s front-end definition phase. The first 5-15% of project effort spent on scope definition—decisions like batch versus continuous flow, isolator footprint, and integration points—irreversibly dictates 75-90% of the final lifecycle cost and operational capability. Getting this foundation right is paramount.
Core Design Principles in Practice
The following table summarizes the key design principles that underpin a modern, compliant ISO Class 5 vial filling line.
| Design Principle | Key Metric / Characteristic | Technology / Method |
|---|---|---|
| Sterility Assurance Level | Highest level | Positive pressure isolator |
| Aseptic Core Environment | ISO Class 5 | Laminar Airflow (LAF) |
| Bio-decontamination Cycle | Validated VHP cycle | Automated decontamination |
| Critical Project Effort | 5-15% initial scope | Defines 75-90% lifecycle cost |
| Material Transfer | Seamless, sterile | Rapid Transfer Ports (RTPs) |
Source: EU GMP Annex 1: Manufacture of Sterile Medicinal Products. This guideline mandates the use of advanced barrier systems and unidirectional airflow to protect the exposed product, directly informing the design principles of isolators and ISO class environments for aseptic filling.
Key Validation Protocols for Aseptic Filling Equipment
Process Simulation: The Ultimate Challenge
Validation provides the documented evidence that an aseptic filling line operates consistently and safely. The cornerstone is the Media Fill or Process Simulation. Here, a sterile growth medium is filled using the standard process, maximum intervention schedule, and longest allowable run time. The filled units are incubated and inspected for microbial growth. Multiple consecutive successful runs with zero contamination are required to prove the aseptic process is under control. This test challenges the entire system—equipment, procedures, and personnel—and is a non-negotiable prerequisite for licensure.
Equipment and Environment Qualification
The Media Fill is supported by rigorous equipment and environmental qualifications. Isolator Decontamination Cycle Validation uses biological indicators placed at worst-case locations to prove a defined log reduction (e.g., 6-log) is consistently achieved. Airflow visualization studies (smoke studies) qualify the unidirectional LAF pattern within the ISO Class 5 zone. Equipment Performance Qualification (PQ) tests filling accuracy, precision, stopper placement, and integrated system functionality under worst-case conditions. Industry experts recommend designing these protocols to not just meet, but exceed, the minimum requirements of EU GMP Annex 1 to build regulatory confidence.
The Data Integrity Imperative
Modern validation extends beyond physical tests to encompass data integrity. Equipment must generate a data-rich environment with Process Analytical Technology (PAT) and strict adherence to 21 CFR Part 11 and ALCOA+ principles. This data integrity is the new currency for regulatory compliance. It enables robust, science-based batch release decisions worth millions of dollars and meets Annex 1 expectations for continuous process verification. A validated system that cannot assure data integrity is a critical compliance liability.
| Protocol | Key Requirement / Metric | Critical Output |
|---|---|---|
| Media Fill (Process Simulation) | Zero contamination | Sterility assurance proof |
| Isolator Decontamination Validation | 6-log reduction (example) | Biological indicator kill |
| Airflow Visualization | Smoke study qualification | Unidirectional LAF pattern |
| Equipment Performance Qualification | Filling accuracy & precision | System functionality proof |
| Data Integrity | 21 CFR Part 11 compliance | Robust batch release |
Source: EU GMP Annex 1: Manufacture of Sterile Medicinal Products. Annex 1 provides the foundational requirements for validation, including process simulation, environmental monitoring, and equipment qualification, which are essential for demonstrating aseptic process control.
Aseptic Filling Equipment: Cost and ROI Considerations
Understanding the Capital Drivers
The capital investment for an aseptic filling line is significant, driven by three primary factors: advanced barrier technology (isolator vs. RABS), precision engineering of filling mechanisms, and the rigor of the validation lifecycle. The choice of isolator technology commands a higher initial investment than a RABS. However, this cost analysis must be lifecycle-based. The higher upfront cost of an isolator is offset by lower long-term operational risk, reduced environmental monitoring burden, and higher sterility assurance, which minimizes the catastrophic cost of a contaminated batch.
Calculating True Return on Investment
ROI extends far beyond equipment purchase price. It encompasses validation timelines, operational flexibility, and regulatory compliance speed. Strategic investment in equipment with superior data integrity and PAT features is essential for efficient batch release, avoiding costly regulatory delays or observations. Furthermore, the industry trend toward modular equipment designs allows for compressed deployment timelines. This agility enables a faster response to public health emergencies and improves ROI by accelerating time-to-market—a critical factor in vaccine capital planning.
| Cost/ROI Factor | Primary Driver | Strategic Impact |
|---|---|---|
| Capital Investment | Barrier technology choice | Isolator vs. RABS cost |
| Operational Risk | Sterility assurance level | Long-term compliance cost |
| ROI Acceleration | Modular equipment design | Faster time-to-market |
| Regulatory Efficiency | Data integrity features | Avoids batch release delays |
| Deployment Timeline | Vendor modularity | Compressed project schedule |
Source: Technical documentation and industry specifications.
Which Filling System Is Better for Your Vaccine Platform?
Matching Technology to Product Profile
The optimal filling system is dictated by the vaccine platform’s specific sensitivity and viscosity. For sensitive biologics like mRNA, lipid nanoparticles (LNPs), or viral vectors, peristaltic pumps with single-use fluid paths are non-negotiable. They minimize shear stress that can degrade product and eliminate cross-contamination risk between batches. For more traditional inactivated or subunit vaccines, highly accurate rotary piston pumps may offer superior precision and speed. The strategic implication is clear: fill/finish flexibility is mandatory for pipeline diversity. A dedicated line for a single platform creates operational inflexibility.
The Case for Modular Multi-Format Platforms
Equipment must handle various container types (2-100mL vials, syringes, cartridges) with quick, validated changeovers. Investing in a modular, multi-format platform is essential for R&D and commercial facilities managing varied pipelines. This adaptability is a core competitive advantage. It allows a single line to support clinical manufacturing through to commercial production for multiple products, maximizing asset utilization. When evaluating systems, prioritize vendors whose designs enable this flexibility without compromising sterility assurance.
Comparing Isolator vs. RABS Technology for Vaccine Lines
Defining the Technological Divide
The choice between an Isolator and a Restricted Access Barrier System (RABS) is a fundamental design decision. Isolators are fully sealed enclosures with automated bio-decontamination cycles (e.g., VHP), providing the highest level of separation from operators. RABS are hard-walled barriers with glove ports but are opened for major interventions, manual cleaning, and setup. According to the standard ISO 13408-6, isolator systems are designed to maintain a defined environment through continuous isolation, which is the basis for their superior classification.
Strategic Implications for Vaccine Production
For vaccine production, especially for live-attenuated or high-containment products, isolators are becoming the regulatory and industry standard. They offer superior sterility assurance, can be maintained at negative pressure for product containment, and align with regulatory preferences for reduced human intervention. While RABS are an accepted technology, they inherently carry a higher risk profile due to operator dependency. The strategic implication for new facilities is to default to isolator technology. This decision future-proofs operations against evolving regulatory expectations and achieves a higher, more defensible sterility assurance level.
| Feature | Isolator | RABS |
|---|---|---|
| Enclosure & Access | Fully sealed, automated | Hard-walled, openable |
| Decontamination Method | Automated VHP cycle | Manual cleaning |
| Sterility Assurance Level | Highest, minimal intervention | High, operator-dependent |
| Pressure Control | Positive or negative | Typically positive |
| Regulatory Alignment | Preferred for new facilities | Accepted, higher intervention |
Source: ISO 13408-6: Aseptic processing of health care products — Part 6: Isolator systems. This standard specifies the design, qualification, and control requirements for isolator systems, providing the technical basis for their superior separation and decontamination capabilities compared to other barrier systems.
Integrating Lyophilization: Critical Design and Validation Steps
Maintaining Sterility at the Transfer Interface
For lyophilized vaccines, the integration between the filler and the freeze-dryer is a critical control point. The design must maintain ISO Class 5 conditions during the transfer of partially stoppered vials from the isolator to the lyophilizer chamber. This is often achieved using HEPA-filtered transfer carts or, more effectively, automated loading/unloading systems (ALUS) that dock directly with both the isolator and lyophilizer. The sterile boundary must remain unbroken throughout this transfer, a challenge that requires meticulous engineering and validation.
Validating the Lyophilization Process
Validation must cover multiple aspects. First, the sterility of the transfer process itself must be challenged, often via media simulation. Second, the lyophilizer’s sterilization-in-place (SIP) cycles must be validated to prove consistent bioburden reduction. Third, the maintenance of critical conditions (temperature, pressure) within the chamber during the cycle must be qualified. Lyophilization is a major throughput bottleneck. Technologies that enable cycle optimization, such as controlled nucleation, are valuable for improving throughput and consistency. Furthermore, sustainability pressures are targeting this energy-intensive process. Equipment with lower carbon and water footprints is becoming a strategic differentiator for meeting corporate ESG goals and may influence supplier selection.
| Integration Aspect | Critical Design Feature | Validation Focus |
|---|---|---|
| Sterile Transfer | HEPA-filtered carts/ALUS | Transfer process sterility |
| Lyophilizer Sterilization | SIP cycles | Chamber bioburden reduction |
| Process Bottleneck | Cycle optimization tech | Throughput validation |
| Environmental Impact | Energy & water footprint | ESG compliance data |
| Chamber Conditions | Parameter maintenance | Critical process parameters |
Source: Technical documentation and industry specifications.
Operational Considerations: Maintenance, Changeover & Staffing
Ensuring Sustained Performance
Sustained operation requires robust, procedurally controlled maintenance and changeover. Changeover procedures between different products or container formats, including parts replacement (e.g., pump heads, stopper bowls) and decontamination, must be rigorously validated to prevent mix-up or contamination. Effective preventive maintenance planning is crucial to minimize unplanned downtime and, just as importantly, to ensure the continuous data integrity of the line’s sophisticated control systems. A single sensor failure can invalidate a batch’s environmental data.
The Evolution of the Operator Role
The pervasive integration of robotics and isolators is fundamentally shifting the required skill set in the cleanroom. The operator’s role is evolving from a manual aseptic technique expert to a system overseer. New competencies in mechatronics, robotics programming, and data system management are essential. Foundational aseptic technique remains critical, but it is now augmented by automation. Strategic workforce development must pivot to emphasize these technical competencies. Training programs based on standards like USP General Chapter <797> provide a strong foundation in aseptic principles, but must be expanded to include advanced equipment operation.
| Operational Area | Key Requirement | Evolving Skill Set |
|---|---|---|
| Changeover Procedures | Rigorously validated | Prevents mix-up/contamination |
| Maintenance Planning | Minimizes downtime | Ensures data integrity |
| Operator Role | System overseer | Mechatronics, robotics |
| Staffing Development | Technical competencies | Data system management |
| Aseptic Technique | Foundational | Augmented by automation |
Source: USP General Chapter <797> Pharmaceutical Compounding—Sterile Preparations. While focused on compounding, this standard underscores the critical importance of personnel training, aseptic technique, and environmental control, principles that translate to the operational rigor required for commercial aseptic filling lines.
Selecting the Right Aseptic Filling Line: A Decision Framework
A Multi-Faceted Evaluation
Selecting the appropriate line requires a structured, multi-faceted decision framework. First, clearly define the primary vaccine platform(s) and container formats. This determines non-negotiable technical specs like pump type, temperature control needs, and containment requirements. Second, evaluate the sterility assurance strategy. For new projects, strongly favor isolator-over-RABS technology to achieve higher assurance and regulatory alignment. Third, assess the supplier’s capability for modularity and rapid deployment to ensure project agility and scalability.
Prioritizing Data and Partnership Models
Fourth, prioritize equipment with inherent data integrity and PAT features. This is no longer a luxury but a core requirement for regulatory compliance and efficient batch release. Fifth, honestly assess operational scalability and the availability of specialized CDMO partners. For many innovators, partnering with a CDMO that has proven expertise in complex platforms like mRNA can be more strategic than building in-house capacity. This model provides access to validated, state-of-the-art vial filling and lyophilization technology without the capital outlay and timeline. Such partnerships, especially with CDMOs possessing surge capacity, act as a critical buffer for health security and de-risk supply chains.
The core decision points are irrevocable: isolator technology for superior sterility, modularity for pipeline agility, and data integrity for compliance. These choices define operational capability for the lifecycle of the facility. Misalignment at this stage creates persistent technical debt and risk.
Need professional guidance to navigate these critical decisions for your vaccine platform? The team at QUALIA specializes in translating complex technical requirements into executable, compliant filling line strategies. Contact us to discuss your project’s specific challenges and timeline.
Frequently Asked Questions
Q: How do you validate the sterility of an isolator-based aseptic filling line?
A: Validation requires a multi-faceted approach, starting with a Media Fill to simulate the process and challenge operator interventions. This is supported by Isolator Decontamination Cycle Validation using biological indicators to prove a defined log reduction, and Environmental Monitoring to qualify the ISO Class 5 zone. These protocols align with the principles for sterile manufacturing in EU GMP Annex 1. For regulatory compliance, you must plan for multiple consecutive successful runs with zero contamination to support batch release.
Q: What are the critical design factors when choosing between an isolator and a RABS for a new vaccine line?
A: The decision hinges on required sterility assurance and operational workflow. Isolators are fully sealed with automated bio-decontamination, offering superior separation and are ideal for high-containment products. RABS are hard-walled but require opening for major interventions. For new facilities, isolator technology is the strategic default to meet regulatory preferences and future-proof operations. This means projects prioritizing the highest sterility assurance should expect a higher initial capital investment for an isolator to secure lower long-term operational risk.
Q: Which filling pump technology is best for sensitive mRNA vaccine platforms?
A: For shear-sensitive products like mRNA, peristaltic pumps with single-use fluid paths are the preferred choice. This technology minimizes stress on the product and eliminates cross-contamination risk between batches. If your pipeline includes diverse vaccine platforms, you should prioritize equipment with this flexibility over dedicated piston-pump systems to maintain operational agility and support pipeline diversity.
Q: How does integrating a lyophilizer impact the design and validation of a filling line?
A: Integration creates a critical control point for maintaining sterility during transfer. The design must preserve ISO Class 5 conditions, often using HEPA-filtered transfer carts or automated loading systems. Validation must then cover the sterility of this transfer and the lyophilizer’s own sterilization cycles. For facilities producing lyophilized vaccines, you must plan for this complex interface validation early, as it is a major throughput bottleneck and a focal point for sustainability improvements.
Q: What operational skill sets are now required for staff managing a modern, automated filling line?
A: The required competencies are shifting from manual aseptic technique to technical oversight. Operators now need skills in mechatronics, robotics programming, and managing the data systems that ensure 21 CFR Part 11 compliance. This evolution is driven by the pervasive integration of isolators and robotics. For strategic workforce development, you should prioritize training in these technical domains to effectively oversee automated systems and maintain continuous data integrity.
Q: What is the most significant cost and timeline driver when implementing a new aseptic filling line?
A: The most impactful decisions are made during the initial scope definition, which dictates 75-90% of the final lifecycle cost. Key early choices include selecting batch versus continuous flow and committing to isolator technology. Furthermore, opting for modular equipment designs from vendors can compress deployment timelines. This means for projects needing a fast response, you should prioritize modularity and supplier agility in your selection criteria to accelerate time-to-market and improve ROI.
Q: How do regulatory standards specifically guide the use of isolator systems in aseptic processing?
A: Isolator design and operation are governed by dedicated standards that provide requirements for qualification and control. The key reference is ISO 13408-6, which covers isolator systems for aseptic processing. This standard works in conjunction with broader sterile product guidelines like EU GMP Annex 1. When validating your system, you must ensure your decontamination cycles and operational procedures meet the specific log reduction and control expectations outlined in these documents.
Related Contents:
- Aseptic Solutions for Sterility Test Isolators
- Biosafety Isolators: Vaccine Production Essentials
- Transfer Chambers in Sterility Test Isolators
- Sterility Test Isolators: Aseptic Isolation Systems
- Aseptic Techniques in OEB4/OEB5 Isolators: User Training
- Maintaining Aseptic Conditions in Test Isolators
- Sterility Test Isolators for Pharmaceutical Products
- Medical Device Testing in Sterility Isolators
- Sterility Testing Assurance: Isolator Technology