Developing vaccines against high-consequence pathogens presents a unique regulatory and scientific challenge. Human efficacy trials are often impossible or unethical, forcing developers to rely on robust preclinical data. The quality of this data hinges on the capabilities of specialized containment facilities. This reliance on animal models for definitive proof of efficacy creates a critical dependency on high-containment research infrastructure.
The strategic importance of these facilities has never been greater. With emerging infectious diseases and biosecurity threats, the ability to rapidly and credibly test vaccine candidates is paramount. Animal Biosafety Level 3 (ABSL-3) laboratories are not just research spaces; they are essential regulatory assets. Their operational and scientific rigor directly determines whether a vaccine candidate can advance to licensure under frameworks like the FDA’s Animal Rule.
The Role of Animal BSL-3 Labs in Regulatory Pathways
Defining the Regulatory Imperative
For pathogens like anthrax, Ebola, or novel respiratory viruses, traditional Phase 3 human trials are not feasible. Regulatory bodies have established pathways, most notably the U.S. FDA’s “Animal Rule,” to address this. This rule permits vaccine approval based on adequate and well-controlled animal studies when human challenge trials are unethical. The mandate is clear: demonstrate efficacy in at least one well-characterized animal species with study endpoints, like survival, that are reasonably likely to predict human benefit.
From Data to Dossier
This regulatory framework transforms animal BSL-3 data from supportive evidence into the primary currency for approval. The studies conducted within these walls carry the definitive weight of a Phase 3 trial. Consequently, the entire development program for an Animal Rule product is architected around generating this preclinical efficacy package. The facility’s compliance with Good Laboratory Practice (GLP) standards, as defined in 21 CFR Part 58 Good Laboratory Practice for Nonclinical Laboratory Studies, becomes non-negotiable for regulatory acceptance.
A Foundational Strategic Asset
This elevates the BSL-3 animal lab from a cost center to a core strategic asset. Its capability to produce reproducible, GLP-compliant data under high containment is a significant barrier to entry and a decisive competitive advantage. In my experience, the most successful programs treat BSL-3 study design with the same strategic forethought as clinical trial design, recognizing its pivotal role in the regulatory dossier.
Core Applications for Vaccine Efficacy and Safety Testing
The Controlled Challenge Paradigm
The definitive application of an animal BSL-3 lab is controlled challenge studies. Vaccinated animals are exposed to the live, virulent pathogen under strict containment to measure protective efficacy. This goes beyond observing symptoms; it involves quantifying survival rates, viral/bacterial load reduction, and pathological changes. The goal is to generate a clear, dose-dependent protection curve that establishes the vaccine’s potency.
The Criticality of Model Selection
No single animal model suffices for all pathogens. Selection is based on which species most accurately replicates human disease pathology and immune response. This requires maintaining a diverse and validated portfolio of models, each with specialized housing and handling protocols. The choice directly impacts study credibility and regulatory acceptance for a specific pathogen program.
The table below illustrates the model-specific approach required for different high-consequence pathogens.
| Pathogen | Primary Animal Model(s) | Key Challenge Route |
|---|---|---|
| Anthrax | Rabbits, Non-human primates | Aerosolized spores |
| Plague | Murine models (mice) | Not specified |
| Respiratory Viruses (e.g., SARS-CoV-2) | Ferrets | Relevant physiological model |
Source: Technical documentation and industry specifications.
Standardization for Reproducibility
A common oversight is underestimating the need for model standardization. The challenge strain, inoculum dose, and administration route must be meticulously controlled and documented to ensure reproducible disease. Variability here introduces noise that can obscure a vaccine’s true efficacy signal, potentially derailing a candidate based on flawed experimental execution rather than scientific merit.
Immunogenicity and Correlate of Protection Studies
Beyond Survival: Dissecting the Immune Response
While survival is the ultimate endpoint, understanding why a vaccine protects is crucial for development. BSL-3 studies enable detailed immunogenicity profiling post-vaccination and challenge. Researchers measure neutralizing antibody titers, T-cell responses, and mucosal immunity. Passive transfer studies—administering serum from vaccinated animals to naïve ones before challenge—are a powerful tool to isolate the protective components of the immune response.
The Quest for Correlates
The strategic goal is to identify an immunologic correlate of protection (CoP). A CoP is a measurable immune parameter, like a specific antibody titer, that predicts protection in the animal model and, by extension, in humans. Establishing a validated CoP is transformative; it allows future candidates to be screened based on immunogenicity data, potentially reducing the number of costly and complex challenge studies needed.
The following table outlines key study types used to unravel protective immunity.
| Study Type | Primary Goal | Strategic Benefit |
|---|---|---|
| Humoral/Cell-mediated immunity measurement | Post-vaccination/challenge immune response | Elucidate protective mechanisms |
| Passive transfer studies | Identify protective mechanisms | Link animal data to human outcomes |
| Correlate of Protection (CoP) identification | Specific antibody titer prediction | Predict human vaccine efficacy |
| Innovative assay development (e.g., heat-inactivated virus) | Transfer testing to BSL-2 | Reduce costs, accelerate workflows |
Source: Technical documentation and industry specifications.
Workflow Innovation within Containment
A key advancement is developing assays that allow critical immunogenicity testing to be transferred from BSL-3 to BSL-2. For instance, using heat-inactivated virus or recombinant proteins for ELISA or neutralization assays enables high-throughput immune monitoring without the constant need for high-containment work. This strategic decoupling accelerates timelines and reduces costs without compromising data integrity.
Optimizing Vaccine Dose and Administration in BSL-3 Models
The Dose-Response Relationship
BSL-3 containment is essential for establishing the vaccine’s dose-response curve. Dose-ranging studies identify the minimum effective dose and the dose at which protection plateaus, informing human dosing strategy. Similarly, comparing administration routes—intramuscular versus intranasal, for example—can reveal stark differences in the magnitude and quality of protection, especially for mucosal pathogens.
Constraints Dictate Design
These optimization studies are heavily constrained by BSL-3 operational bottlenecks. Stringent PPE, limited time in containment suites, and complex sample inactivation procedures restrict the number of animals that can be handled and the frequency of sampling. This directly impacts statistical power. Therefore, study design must be optimized for logistical efficiency from the outset, often using fractional factorial designs to extract maximum information from minimal animal cohorts.
The Schedule and Formulation Variable
Determining the optimal prime-boost interval and evaluating different vaccine formulations (e.g., with various adjuvants) are further applications. Each variable tested multiplies the number of experimental groups, exacerbating logistical challenges. The most effective programs use pilot studies in smaller, more manageable models to narrow down options before committing to definitive studies in larger, more relevant species.
Operational Challenges and Technical Considerations
The Physical and Procedural Bottleneck
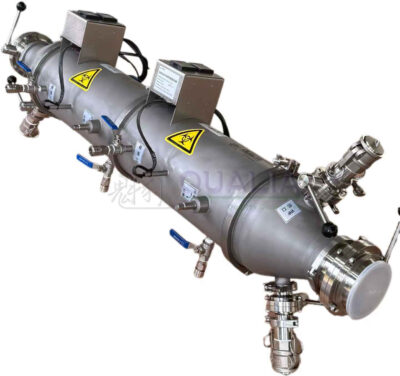
Work in an ABSL-3 environment is conducted within primary containment devices like Class III biosafety cabinets or isolators, with rigid negative airflow controls. Extensive PPE (respirators, double gloves, Tyvek suits) limits dexterity, visibility, and work duration. Every material entering or exiting requires decontamination, often via autoclave or chemical dunk tanks, creating significant workflow friction.
The Scale and Cost Dilemma
These constraints severely limit scale. Group sizes, especially for large animals like non-human primates (NHPs), are often smaller than ideal due to space, cost, and handling complexity. The per-animal cost in a BSL-3 NHP study is an order of magnitude higher than in conventional research. This economic reality forces tough trade-offs between statistical rigor and project budget.
The operational matrix below details the primary constraints and their impacts.
| Constraint Category | Specific Challenge | Impact on Research |
|---|---|---|
| Physical Containment | Class III cabinets, isolators | Limits work dexterity, duration |
| Safety Procedures | Rigid airflow controls, waste inactivation | Reduces sampling frequency |
| Animal Model Scale | Large animal studies (e.g., NHPs) | Limits group sizes, increases cost |
| Regulatory Compliance | Good Laboratory Practice (GLP) standards | Adds complexity, requires validated assays |
Source: 21 CFR Part 58 Good Laboratory Practice for Nonclinical Laboratory Studies. This regulation sets the quality and integrity requirements for nonclinical studies, directly governing the complex operational layer of GLP compliance within BSL-3 labs that is critical for regulatory acceptance of vaccine data.
The GLP Compliance Layer
For pivotal regulatory studies, GLP compliance adds another dimension of complexity. It requires a dedicated quality assurance unit, validated assays performed within containment, and meticulous, real-time documentation. Mastering the integration of BSL-3 operations, animal expertise, and GLP standards is a rare capability, making specialized CDMOs with this integrated expertise invaluable partners.
Integrating BSL-3 Research into the Development Pipeline
Phase-Specific Objectives
BSL-3 research is not a monolithic activity; it integrates into specific preclinical phases with distinct goals. Early proof-of-concept uses small, cost-effective models like mice or hamsters for rapid screening of multiple vaccine candidates. Lead optimization then employs more sophisticated models, often in two species, to generate comprehensive data on protection and immunogenicity for the lead candidate.
The Pivotal Study
The culmination is the definitive, GLP-compliant efficacy study. This study is designed and executed with regulatory scrutiny as the primary focus, forming the core of the preclinical package for an Investigational New Drug (IND) application. For Animal Rule pathogens, this study is the definitive efficacy evidence, demanding premier resource allocation and oversight.
The integration of these phases into the regulatory pathway is summarized below.
| Preclinical Phase | Primary Animal Models | Key Objective & Regulatory Role |
|---|---|---|
| Early Proof-of-Concept | Mice, hamsters | Candidate vaccine screening |
| Lead Optimization | Two species, sophisticated models | Comprehensive protection/immunogenicity data |
| Definitive Efficacy Studies | GLP-compliant models | IND application support, substitutes for human trials |
Source: 21 CFR Part 58 Good Laboratory Practice for Nonclinical Laboratory Studies. The GLP standards defined here are mandatory for the definitive nonclinical laboratory studies that form the critical preclinical package for an Investigational New Drug (IND) application to regulatory bodies like the FDA.
A Strategic, Not Tactical, Activity
The key is to establish the validated animal model early. Treating BSL-3 studies as a tactical box to check late in development is a high-risk strategy. The model must be characterized, and challenge standards established during lead optimization to de-risk the pivotal study. This proactive integration ensures the BSL-3 data package is robust, reproducible, and ready for regulatory submission.
Future Directions and Emerging Pathogen Preparedness
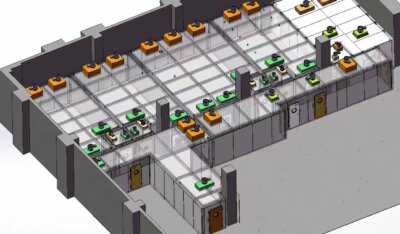
Modularization and Accessibility
The future of pandemic preparedness hinges on agile, accessible BSL-3 capacity. Pre-fabricated, modular BSL-3 laboratories represent a disruptive strategy. They enable rapid deployment and scaling of containment infrastructure, which is crucial for establishing regional response capabilities and addressing global health equity. This trend supports decentralized research and development networks.
Agile Manufacturing Networks
This aligns with a broader shift toward distributed, agile manufacturing. The future model combines modular BSL-3 facilities with platform vaccine technologies (mRNA, viral vectors) to create regional networks capable of rapid response. The strategic priority is moving from centralized, monolithic production to flexible, geographically dispersed nodes that prioritize speed and resilience over sheer scale.
Platform Validation
A critical forward-looking activity is the pre-validation of animal models for platform technologies. Demonstrating that a particular model (e.g., ferrets for mRNA vaccines against respiratory viruses) is predictive across a class of pathogens can significantly accelerate response times for novel threats using the same platform, turning the BSL-3 lab into a true preparedness asset.
Selecting Models and Designing Effective BSL-3 Studies
The Model Selection Trilemma
Effective study design begins with strategic model selection, balancing three factors: physiological relevance to human disease, regulatory precedent for the pathogen, and practical constraints (cost, availability, BSL-3 handling suitability). For respiratory pathogens, the ferret model is particularly strategic. It is a cost-effective, physiologically relevant non-rodent species that can fulfill the FDA’s expectation for data in two animal species for certain applications.
Standardization and Endpoint Definition
Once a model is selected, study design focuses on standardization. The challenge strain must be clinically relevant and banked. The challenge dose and route are calibrated to produce consistent, measurable disease without overwhelming mortality. Clinical scoring systems and precise immunological endpoints (e.g., viral titer in lung tissue at day 5 post-challenge) must be defined prospectively.
The framework below outlines critical design considerations for BSL-3 studies.
| Design Factor | Key Consideration | Example/Impact |
|---|---|---|
| Model Selection Criteria | Physiological relevance, regulatory precedent | Ferrets for respiratory pathogens |
| Strategic Model Advantage | Cost-effective, non-rodent species | Fulfills FDA “two-animal rule” |
| Study Standardization | Challenge strain, dose, and route | Reproducible disease pathology |
| Operational Constraint | Logistical and budgetary limits | Favors smaller models for screening |
Source: Technical documentation and industry specifications.
Designing for Constraint
The final, often underestimated, step is designing the study within the harsh realities of BSL-3 logistics. This means powering the study appropriately despite smaller group sizes, simplifying sample collection schedules to minimize time in PPE, and building redundancy into critical procedures. A well-designed BSL-3 study is as much a feat of operational planning as it is of scientific inquiry.
The decision to advance a vaccine candidate against a high-consequence pathogen rests on the integrity of BSL-3 animal data. Prioritize establishing a validated animal model early in development, as this model will generate the definitive efficacy evidence for regulators. Integrate GLP compliance and operational logistics into the study design phase, not as an afterthought. Finally, view the BSL-3 function not as a service but as a core strategic capability that determines program viability.
Need professional support navigating the complex intersection of high-containment research and regulatory strategy? QUALIA provides integrated expertise to de-risk your vaccine development pipeline. Our approach ensures your preclinical data meets the highest standards of scientific and regulatory rigor.
Frequently Asked Questions
Q: How do animal BSL-3 studies fit into the regulatory approval process for vaccines against high-consequence pathogens?
A: They provide the pivotal preclinical efficacy data required under regulatory frameworks like the FDA’s Animal Rule, which is used when human challenge trials are unethical. This rule mandates demonstrating protection in at least one well-characterized animal model, making these studies a direct substitute for Phase 3 human trials for certain pathogens. This means your development program for agents like anthrax or Ebola must prioritize generating robust, reproducible animal data as the primary currency for licensure, governed by standards like 21 CFR Part 58.
Q: What are the key operational bottlenecks when designing vaccine dose-ranging studies in a BSL-3 environment?
A: The primary constraints are the stringent PPE, decontamination protocols, and physical containment, which severely limit the number of animals you can handle and the frequency of sampling. These logistical hurdles directly impact statistical power and data quality. For projects where dose optimization is critical, you must design studies for maximum efficiency from the outset, as operational limitations can compromise results more than scientific methodology if not meticulously planned.
Q: Why is selecting the right animal model a strategic decision for BSL-3 vaccine research?
A: No single species reliably mimics human disease for all pathogens, so model selection directly impacts study credibility and regulatory acceptance. Your portfolio must be pathogen-specific: ferrets for respiratory viruses, non-human primates for anthrax, and murine models for plague. This strategic requirement forces an investment in maintaining diverse, validated models and their associated containment protocols, which is a significant cost and expertise barrier.
Q: How can immunogenicity testing be accelerated within the constraints of high-containment work?
A: A key strategy is developing innovative assays, such as those using heat-inactivated virus, that allow critical immune monitoring to be transferred from BSL-3 to lower-containment BSL-2 labs. This reduces costs and accelerates workflows without compromising safety. If your program requires frequent immunogenicity readouts, you should plan for this assay development early to alleviate operational bottlenecks and streamline your research pipeline.
Q: What makes integrating Good Laboratory Practice (GLP) standards into BSL-3 operations particularly challenging?
A: It creates a trifecta of complexity by combining the inherent physical constraints of containment, the rigorous documentation and quality assurance mandates of GLP, and the need for specialized animal expertise. This high barrier to entry makes mastering this integration a rare capability. For organizations without dedicated infrastructure, partnering with a CDMO that has proven competency in this area is often a necessary strategic decision to ensure data integrity for regulatory submissions under 21 CFR Part 58.
Q: What is the strategic value of the ferret model in respiratory vaccine development?
A: Ferrets offer a cost-effective, physiologically relevant non-rodent model that can fulfill regulatory requirements for demonstrating efficacy in two animal species for certain pathogens. Their relevance to human respiratory disease makes them invaluable for early screening and lead optimization. This means for programs targeting influenza or coronaviruses, the ferret model should be a cornerstone of your preclinical strategy to generate compelling data before committing to pivotal NHP studies.
Q: How do modular BSL-3 laboratories address future pandemic preparedness needs?
A: Pre-fabricated, modular labs offer a strategy for rapid, cost-effective deployment, enabling lab expansion or establishment in diverse geographic settings. This supports decentralized research and vaccine production capabilities. For global health initiatives prioritizing regional self-sufficiency and rapid response, investing in such agile, distributed manufacturing networks is becoming a critical strategic direction over relying solely on centralized facilities.
Related Contents:
- Vaccine Development in BSL-3 Labs: Latest Studies
- Zoonotic Disease Studies in BSL-3 Labs: Insights
- BSL-4 Animal Research: Ensuring Handler Safety
- Vaccine Development in BSL-4 Labs: From Bench to Trials
- BSL-3 Animal Housing: Safe Containment Systems
- Zoonotic Diseases: BSL-4 Lab Investigations Revealed
- BSL-3 Biodefense: Pioneering Research Projects
- How to Size Bioreactors for mRNA Vaccine Production: Cell Culture Volume Calculator
- BSL-3 Animal Research: Facility Design Guide