Selecting the correct biosafety equipment configuration is a high-stakes decision for laboratory managers. The choice between BSL 2, 3, and 4 systems directly impacts capital budgets, operational workflows, and, most critically, personnel safety. A common misconception is that biosafety level is determined solely by the pathogen list, leading to costly over-containment or dangerous under-protection.
The evolving regulatory landscape and the need to manage emerging pathogens with unknown risks make a strategic, risk-based framework essential. This decision requires moving beyond a simple checklist to a holistic analysis of procedures, validation requirements, and total cost of ownership.
BSL 2 vs BSL 3 vs BSL 4: Defining the Core Differences
The Escalation of Containment Principles
The fundamental distinction between Biosafety Levels lies in the escalating combination of practices, safety equipment, and facility safeguards required to mitigate increasing risk. BSL-2 manages moderate-risk agents, relying on proper biosafety cabinet (BSC) use and PPE. BSL-3 is for serious, potentially aerosol-transmitted agents, mandating enhanced engineering controls like negative air pressure and HEPA-filtered exhaust. BSL-4 is reserved for the most dangerous exotic agents, utilizing either sealed Class III BSCs or positive-pressure supplied-air suits.
Activity-Driven, Not Just Agent-Driven
A critical, often overlooked detail is that BSL level is activity-driven. For instance, routine diagnostic testing for a BSL-3 agent can often be performed at BSL-2, while viral culture of the same agent requires BSL-3 containment. This decoupling means decisions must be based on robust, site-specific risk assessments evaluating aerosol potential and exposure consequences, not just pathogen names. Industry experts recommend mapping every procedure, from pipetting to sonication, to identify the true containment requirement.
The Strategic Implication for Configuration
This procedural focus creates strategic flexibility. Implementing validated sample inactivation methods can act as a procedural gateway, allowing materials to be safely analyzed at a lower BSL. This approach can provide access to specialized equipment located in standard labs without compromising safety, a key consideration for maximizing facility utility.
Cost Comparison: Capital, Operational, and TCO Analysis
Understanding the Financial Escalation
The financial commitment escalates dramatically with each BSL, impacting capital expenditure (CapEx), operational costs (OpEx), and total cost of ownership (TCO). BSL-2 primarily involves BSCs and basic PPE. BSL-3 requires significant facility overhaul for directional airflow and HEPA filtration. BSL-4 represents a monumental investment in a structurally independent zone with redundant, complex systems. According to industry analysis, the largest cost driver shifts from equipment at BSL-2 to facility engineering at BSL-3 and 4.
Strategic Capital Planning and Flexibility
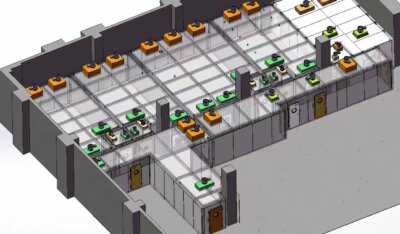
Capital planning must follow the engineering control hierarchy, prioritizing primary containment devices like BSCs. A pivotal strategic insight is designing flexible BSL-2 spaces with infrastructure that can support enhanced protocols—such as capacity for additional BSCs or potential for directional airflow. This can delay the massive capital outlay for a full BSL-3 build-out, creating a strategic hybrid zone for managing emerging pathogen research or diagnostic surges. We compared planning approaches and found this “BSL-2 plus” design significantly improves long-term adaptability.
Comparative Cost Breakdown
The following table provides a high-level comparison of key cost components across biosafety levels, illustrating the shift in financial burden.
| Componente de custo | BSL-2 | BSL-3 | BSL-4 |
|---|---|---|---|
| Primary Capital (BSCs) | Class I/II BSCs | Sophisticated Class II BSCs | Class III BSC line / Suit Lab |
| Facility Engineering | Basic benches, sinks | Negative pressure, HEPA exhaust | Structurally independent zone |
| Sistema de descontaminação | Access to autoclave | On-site autoclave suite | Redundant, validated systems |
| Complexidade operacional | Annual BSC certification | Enhanced PPE, rigorous training | Specialized suit maintenance |
Source: Technical documentation and industry specifications.
Primary Containment: BSC Requirements Compared by BSL
The Central Role of the BSC
Primary containment centers on the Biological Safety Cabinet, with requirements scaling directly with risk. At BSL-2, a Class I or II BSC is required for aerosol or splash potential. BSL-3 mandates all work with infectious materials be conducted within a Class II BSC or similar device. BSL-4 offers two models: absolute containment via a Class III BSC line or the use of Class II BSCs within a positive-pressure suit environment. The defining boundary for requiring a BSC is aerosol generation.
Procedure-Specific Mandates
Procedures like vortexing, pipetting, or sonication mandate primary containment within a BSC, regardless of the nominal BSL. A common mistake is assuming open-bench manipulation is permissible at BSL-2 for “low-risk” steps; this is prohibited for any aerosol-generating activity. If a BSC is unavailable, a combination of sealed secondary containment and enhanced respiratory protection becomes the minimum requirement, directly linking equipment configuration to procedural risk mapping.
BSC Requirements by Procedure
The requirements are clearly defined by authoritative guidance. The table below, based on the Biossegurança em laboratórios microbiológicos e biomédicos (BMBL) 6ª edição, compares BSC requirements for common laboratory procedures across biosafety levels.
| Work Procedure | BSL-2 Requirement | Requisito BSL-3 | Requisito BSL-4 |
|---|---|---|---|
| Aerosol-generating procedures | In Class I/II BSC | In Class II BSC | In Class III BSC / Suit Lab |
| Open-bench manipulation | Prohibited for aerosols | All work in BSC | Não se aplica |
| Centrifugation | Sealed safety cups | Sealed safety cups | Absolute containment |
| If BSC unavailable | Sealed containment + respirator | Not standard practice | Not permissible |
Source: Biossegurança em laboratórios microbiológicos e biomédicos (BMBL) 6ª edição. The BMBL defines the primary containment barriers required for each biosafety level, specifying the types of Biological Safety Cabinets (BSCs) and physical containment devices necessary for safe operations.
Secondary Containment: Facility and Engineering Control Escalation
The Facility as a Barrier
Secondary containment refers to facility engineering controls, which see a major escalation at BSL-3. BSL-2 labs require basic features like impervious benches and sinks. BSL-3 introduces critical safeguards: negative air pressure, HEPA-filtered exhaust discharged outdoors, and access through an anteroom. BSL-4 facilities are structurally independent with dedicated, redundant supply/exhaust systems and chemical shower decontamination. In my experience, retrofitting these controls into an existing BSL-2 space is often more costly and complex than new construction.
Engineering Control Specifications
The specific requirements for these controls are codified in biosafety standards. The following table outlines the escalation of key engineering controls, as detailed in the Biossegurança em laboratórios microbiológicos e biomédicos (BMBL) 6ª edição.
| Controle de engenharia | BSL-2 | BSL-3 | BSL-4 |
|---|---|---|---|
| Pressão do ar | Nenhum requisito específico | Pressão negativa | Negative pressure, redundant |
| Exhaust Air | Ventilação geral | HEPA-filtered, to outside | Dedicated, redundant HEPA |
| Controle de acesso | Self-closing doors | Anteroom or airlock | Airlock, chemical shower |
| Waste Exit | Reliable decontamination access | In-lab autoclave | Multiple validated effluent systems |
Source: Biossegurança em laboratórios microbiológicos e biomédicos (BMBL) 6ª edição. The BMBL outlines the specific facility safeguards and secondary barriers, such as directional airflow and access provisions, that escalate with each increasing biosafety level.
Workflow Dictated by Waste Streams
A key strategic implication is that integrated waste stream management fundamentally dictates laboratory layout. The requirement to decontaminate all waste before removal creates a critical workflow bottleneck. Efficient design must be reverse-engineered from the waste exit point—whether an autoclave or effluent treatment system—back to the bench. This ensures a safe, logical material flow that maintains both operational continuity and containment integrity, preventing cross-contamination and procedural delays.
PPE and Staffing Requirements: A Comparative Overview
The Last Line of Defense
PPE serves as the final personal defense, with requirements intensifying by BSL. BSL-2 requires lab coats, gloves, and eye protection. BSL-3 necessitates solid-front gowns or coveralls, often with double gloves, and respiratory protection (N95 to PAPR). BSL-4 requires a full-body positive-pressure suit or equivalent. Staffing demands also increase, with BSL-3/4 requiring rigorous, specialized training and higher supervision ratios. Easily overlooked details include the need for formal fit-testing for respirators and suit integrity checks.
A Tiered Hierarchy Within Each BSL
PPE selection follows a tiered hierarchy within each BSL. High-risk BSL-2 work, such as manipulating concentrated stocks, may demand solid-front gowns and N95 respirators. Conversely, lower-risk BSL-3 procedures with validated containment might not require PAPRs. This sub-classification means procurement must move beyond a one-size-fits-all approach, tailoring PPE kits to specific procedural risks identified in the assessment. International standards like ISO 15190:2020 provide a framework for this risk-based selection.
Comparative Overview of PPE and Staffing
The escalation in personal protection and personnel requirements is systematic. The table below compares these key requirements across biosafety levels.
| Requisito | BSL-2 | BSL-3 | BSL-4 |
|---|---|---|---|
| Base Attire | Jaleco de laboratório, luvas | Solid-front gown, double gloves | Full-body positive-pressure suit |
| Proteção respiratória | Eye/face protection | N95 respirator to PAPR | Integrated suit air supply |
| Nível de treinamento | Standard lab safety | Rigorous, specialized training | Extensive, suit-specific training |
| Staffing Supervision | Standard ratios | Higher supervision ratios | Constant, specialized oversight |
Source: ISO 15190:2020 Medical laboratories — Requirements for safety. This standard provides a framework for risk-based selection of personal protective equipment (PPE) and establishes requirements for personnel competence and training, which scale with operational risk.
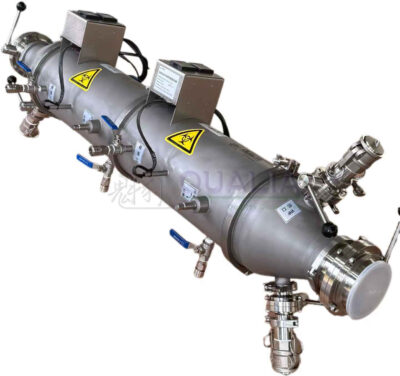
Decontamination and Waste Handling: Equipment by Biosafety Level
Scaling Decontamination Protocols
Decontamination protocols and equipment scale with containment level. BSL-2 requires reliable access to an autoclave. BSL-3 mandates an autoclave within the lab suite, with potential need for liquid effluent treatment. BSL-4 requires redundant, validated systems for all waste streams. A critical shift is occurring in regulatory focus: from assuming performance to demanding empirical proof. This changes decontamination from a supporting activity to a core compliance function.
The Validation Imperative
Regulators increasingly demand validation studies for autoclaves, chemical disinfectants, and fumigants. Laboratories must budget for and conduct regular validation using biological indicators, treating this as a non-negotiable compliance activity. This emphasis on proven methods also enables strategic workflow gates. For example, validated sample inactivation permits safe transfer of materials to lower BSLs for analysis using specialized high-throughput analytical equipment, unlocking greater research or diagnostic capability without compromising safety.
Equipment Requirements by Waste Stream
The specific equipment needs for managing different waste streams escalate significantly. The following table outlines the typical requirements.
| Fluxo de resíduos | BSL-2 | BSL-3 | BSL-4 |
|---|---|---|---|
| Resíduos sólidos | On-site/access to autoclave | Autoclave within lab suite | Redundant validated autoclaves |
| Resíduos líquidos | Desinfecção química | Liquid effluent treatment system | Validated effluent decontamination |
| Resíduos gasosos | Ventilação geral | Filtragem HEPA no escapamento | Descontaminação gasosa completa |
| Validation Focus | Assumed performance | Empirical proof required | Core compliance activity |
Source: Technical documentation and industry specifications.
Which Configuration Is Right for Your Specific Use Case?
Initiate with a Formal Risk Assessment
Selecting the right configuration is a systematic, risk-based process. It begins with identifying the agent and every specific procedure, followed by a formal risk assessment. This assessment must evaluate aerosol potential, exposure consequences, and the availability of post-exposure prophylaxis. The output maps each procedure to primary containment needs and defines supporting equipment like sealed centrifuges or closed-system fermenters.
Navigate Regulatory Dynamics
Managers must be aware that regulatory status can shift requirements mid-process. Identifying a Select Agent or Toxin triggers immediate protocol and containment changes. Laboratories need pre-approved plans for agent transfer and clear, conservative procedures for handling samples of undetermined risk. This dynamic compliance landscape necessitates a management system that is both documented and adaptable.
Leverage Procedural Gateways
The most effective strategy often involves creating procedural gateways using validated inactivation. This risk-management approach allows a single laboratory to operate at multiple effective containment levels based on workflow stage. It optimizes resource use and safety simultaneously, ensuring the highest containment is reserved only for procedures with unmitigated risk.
Implementing Your Decision: A Step-by-Step Procurement Framework
Verify Facility Capability First
Implementation requires a structured approach. The first, non-negotiable step is verifying facility capability. You cannot implement BSL-3 practices in a BSL-2 space. Confirm directional airflow, exhaust treatment capacity, and decontamination infrastructure are physically present and operationally validated. This step prevents the critical error of procuring equipment for a containment level the facility cannot support.
Document Specifications and Validation Plans
Next, formally document the risk assessment and the resulting equipment performance specifications. Concurrently, establish the validation plans for that equipment—biological indicator protocols for autoclaves, annual certification for BSCs, and disinfectant efficacy testing. Procure equipment that is compatible with the containment level, prioritizing primary engineering controls over secondary or administrative solutions.
Institute Protocol-Specific Training
Finally, institute rigorous, protocol-specific training. The future trend points toward protocol-specific, not lab-wide, BSL guidance. Personnel must understand the “why” behind each piece of equipment and PPE requirement for their specific tasks. This demands digital tools to manage dynamic risk assessments for each workflow, moving beyond static facility certifications to demonstrate real-time, procedure-based compliance and competency.
The core decision points hinge on your procedural risk assessment, not a static agent list. Prioritize validating primary containment and decontamination methods, as these form the backbone of your safety case. Design workflows with clear inactivation gateways to maximize operational flexibility while maintaining integrity.
Need professional guidance to navigate your specific biosafety configuration and validation requirements? The experts at QUALIA provide consultative support to translate risk assessments into compliant, efficient laboratory systems. Entre em contato conosco to discuss your project’s requirements.
Perguntas frequentes
Q: How do we determine if a BSL-3 agent requires a full BSL-3 lab or if we can work at BSL-2?
A: The biosafety level is determined by the specific procedure, not just the agent. Diagnostic testing like ELISA for a BSL-3 pathogen can often be done at BSL-2, while activities that generate aerosols, such as viral culture, mandate BSL-3 containment. You must conduct a site-specific risk assessment evaluating aerosol potential and exposure consequences. This means your equipment configuration should be based on a procedural risk map, allowing for cost-effective BSL-2 operations when validated methods permit, as outlined in core risk management principles in ISO 15190:2020.
Q: What is the most significant cost driver when planning an upgrade from BSL-2 to BSL-3 containment?
A: The largest financial hurdle is the overhaul of secondary containment and engineering controls, not primary equipment. Moving to BSL-3 requires installing directional negative air pressure, HEPA-filtered exhaust systems, and often an anteroom or airlock. These facility modifications far exceed the cost of adding more sophisticated biosafety cabinets or PPE. For projects where capital is constrained, you should first invest in flexible BSL-2 infrastructure that can later support enhanced protocols to delay the full BSL-3 build-out.
Q: When is a Biosafety Cabinet absolutely required, and what are the alternatives if one is not available?
A: A BSC is mandatory for any procedure with aerosol or splash potential, such as pipetting, vortexing, or sonication, regardless of the nominal biosafety level. If a BSC is unavailable, the minimum requirement shifts to using sealed secondary containment devices, like safety centrifuge cups, combined with enhanced respiratory protection (e.g., a PAPR). This direct link between procedure and equipment means your risk assessment must explicitly identify all aerosol-generating steps to specify the correct primary containment or PPE combination.
Q: How should we design laboratory workflow to handle BSL-3 waste decontamination efficiently?
A: Efficient design must be reverse-engineered from the waste exit point. The requirement to autoclave waste within the lab suite before removal creates a critical workflow bottleneck. You should plan the laboratory layout so that waste logically flows from the bench to the on-site autoclave, maintaining containment throughout. This means facilities planning an upgrade must prioritize the location and capacity of decontamination equipment early in the design phase to ensure operational continuity and safety.
Q: What is the emerging compliance focus for decontamination equipment like autoclaves in high-containment labs?
A: Regulators now emphasize empirical validation of decontamination efficacy over assumed performance. You must regularly conduct and document validation studies using biological indicators for autoclaves and verify chemical disinfectant protocols. This is a core compliance activity, not an optional check. If your operation requires handling regulated materials, plan to budget for ongoing validation and treat these studies as critical workflow gates that enable safe transfer of inactivated samples to lower BSL areas.
Q: Can we implement BSL-3 work practices in an existing BSL-2 laboratory space?
A: No, you cannot fully implement BSL-3 practices in a BSL-2 facility. The secondary engineering controls are fundamentally different. BSL-3 mandates verified negative air pressure, HEPA-filtered exhaust, and access control through an anteroom, which are typically absent in BSL-2 spaces. This means your first implementation step must be to verify and potentially upgrade the facility’s infrastructure before procuring BSL-3 equipment or beginning work, as defined in the facility design sections of the Biossegurança em laboratórios microbiológicos e biomédicos (BMBL) 6ª edição.
Q: How should we approach PPE procurement for different procedures within the same biosafety level?
A: Move beyond a one-size-fits-all approach by tailoring PPE to specific procedural risks. High-risk BSL-2 work may require solid-front gowns and N95 respirators, while some lower-risk BSL-3 procedures might not need powered air-purifying respirators (PAPRs). This sub-classification requires your risk assessment to map PPE requirements directly to each workflow’s aerosol potential and exposure consequences. For labs with diverse protocols, expect to stock and manage multiple tiers of PPE to match the assessed risk of each activity.
Conteúdo relacionado:
- Estudos de aerossol BSL-3: Práticas seguras de pesquisa
- BSL-3 vs BSL-4: Principais diferenças nos níveis de segurança dos laboratórios
- Centrífugas BSL-3: Recursos avançados de segurança
- Inspeções de segurança BSL-3/4: Lista de verificação abrangente
- Pesquisa com animais BSL-4: Garantindo a segurança do manipulador
- Gerenciamento de resíduos BSL-3: Equipamentos de última geração
- Esterilização de resíduos BSL-4: Como garantir o descarte seguro
- Gerenciamento de resíduos BSL-4: Protocolos para descarte seguro
- Gerenciamento de resíduos BSL-4: Protocolos para descarte seguro