De druk van de regelgeving om de uitstoot van ethyleenoxide (EtO) te verminderen neemt toe, maar een directe overstap naar verdampt waterstofperoxide (VHP) is geen eenvoudige één-op-één vervanging. Contractsterilisatoren staan voor een complexe technische en strategische beslissing: welke apparaten in hun portfolio zijn echt geschikt voor VHP en hoe zorgen ze voor een conforme, efficiënte overgang zonder de service aan de klant in gevaar te brengen? Als dit wordt gezien als slechts een vervanging van het sterilisatiemiddel, bestaat het risico op validatiefouten, materiële schade en operationele verstoring.
Deze overgang is urgent. De wettelijke herclassificatie van VHP als een gevestigde methode en de dreigende beperkingen van de EtO-capaciteit zorgen ervoor dat er steeds minder ruimte is voor strategische actie. Het omschakelingsproces nu onder de knie krijgen is cruciaal om de continuïteit van de toeleveringsketen te behouden, nieuwe marktvraag aan te boren en operationele veerkracht op te bouwen. De omschakeling gaat niet alleen over naleving; het is een fundamentele herwaardering van sterilisatie als bedrijfsactiviteit.
Fase 1: Strategische beoordeling en haalbaarheidsaudit
De levensvatbaarheid van de portefeuille bepalen
De eerste stap is een rigoureuze, gegevensgestuurde audit van uw volledige portfolio EtO-gesteriliseerde hulpmiddelen. Catalogiseer elk item met zijn specifieke constructiematerialen, geometrische complexiteit, verpakkingstype en historische gegevens over bioburden. Deze inventarisatie is niet administratief, maar vormt de technische basis voor alle daaropvolgende beslissingen. Het doel is om te bepalen welke hulpmiddelen succesvol kunnen worden geconverteerd en welke afhankelijk blijven van de unieke materiaalcompatibiliteit en penetratiemogelijkheden van EtO.
Screening op technische beperkingen
Deze audit voert een voorbereidende technische screening uit om items met een hoog risico te markeren. VHP heeft bekende beperkingen met bepaalde oxidatiegevoelige materialen, zoals sommige kleefstoffen, materialen op basis van cellulose en ongecoate metalen zoals koper. De geometrie van het apparaat is even kritisch; lange, smalle lumina (bijv, <1mm diameter and>500 mm lengte) vormen een aanzienlijke penetratie-uitdaging voor de damp. Het belangrijkste is dat de aanwezigheid van organisch vuil een universele sterilisatieblokkering vormt voor zowel EtO als VHP, waardoor effectieve reiniging een absolute voorwaarde is. Uit onze ervaring met procesvalidatie blijkt dat onderschatting van de invloed van grond de meest voorkomende oorzaak is van sterilisatiefouten in nieuwe procesopstellingen.
Strategische portefeuille splitsing
Het resultaat van deze fase is een gesplitste portfoliostrategie. U maakt een duidelijk onderscheid tussen apparaten die geschikt zijn voor VHP-omzetting en apparaten die vanwege technische beperkingen op EtO moeten blijven. Deze duidelijkheid is essentieel voor de toewijzing van middelen en vormt de basis voor de langetermijnplanning. Het benadrukt ook de noodzaak om samen te werken met polymeerleveranciers die innoveren met het oog op VHP-compatibiliteit, waardoor problematische componenten mogelijk opnieuw kunnen worden ontworpen of geformuleerd voor toekomstige conversie.
| Apparaatkenmerk | Risico op verenigbaarheid met VHP | Belangrijkste selectiecriteria |
|---|---|---|
| Type materiaal | Oxidatiegevoelig | Lijmen, ongecoat koper |
| Apparaatgeometrie | Hoog penetratierisico | Lumen <1mm, >500 mm lengte |
| Bioburden en bodem | Universele sterilisatieblokker | Aanwezigheid van organische grond |
| Verpakking | Varieert | Materiaal doorlaatbaarheid |
| Resultaat van de audit | Portefeuille bifurcatie | Geschikt voor VHP vs. EtO vereist |
Bron: Technische documentatie en industriespecificaties.
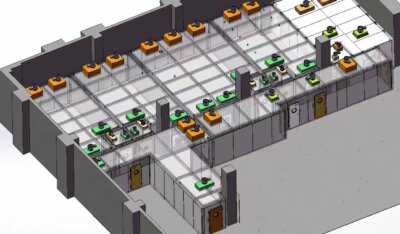
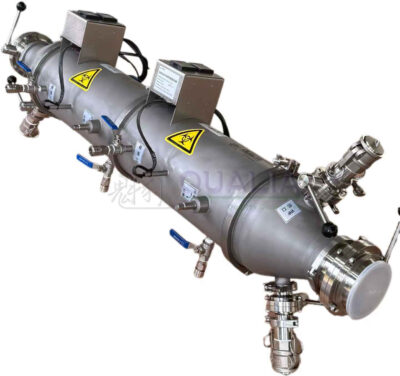
Fase 2: Selectie van het VHP-systeem en faciliteitsplanning
Doorvoer in evenwicht brengen met specificaties
Het selecteren van een VHP-systeem vereist het afstemmen van technische specificaties op commerciële verwerkingsdoelen. Definieer niet-onderhandelbare vereisten voor kamergrootte, cyclustijd en integratie met bestaande materiaalverwerking. Geef de voorkeur aan systemen met geavanceerde, real-time bewakingsmogelijkheden voor kritieke parameters: H₂O₂-dampconcentratie, vochtigheid in de kamer en temperatuur. Deze gegevensintegriteit is essentieel voor validatie en routinecontrole.
Impact van faciliteit beoordelen
Een belangrijk voordeel van VHP komt naar voren in de effectbeoordeling van de installatie. In tegenstelling tot EtO, dat processtoom, complexe gasreductiesystemen en gespecialiseerde gevaarlijke ventilatie vereist, hebben VHP-systemen meestal alleen standaard elektrisch vermogen nodig. Deze drastische vermindering van infrastructuurbelasting voor faciliteiten verlaagt de kapitaaluitgaven en maakt een snellere, flexibelere inzet binnen bestaande footprints mogelijk. De operationele implicaties zijn diepgaand: Het primaire voordeel van VHP is vaak operationeel, niet microbieel.
De belangrijkste zakelijke argumenten
De verschuiving van EtO-cyclustijden van meer dan 14 uur naar VHP-cycli van vaak minder dan 2 uur vertaalt zich direct in een hogere doorvoer, een lagere voorraad onderhanden werk en een grotere flexibiliteit in de toeleveringsketen. Deze efficiëntie vormt de kern van de financiële rechtvaardiging die verder gaat dan naleving van de regelgeving. Bij de evaluatie van systemen moet bij de totale eigendomskosten rekening worden gehouden met deze verwerkingswinst en de verbruikskosten van waterstofperoxide.
| Systeemvereisten | Typische VHP-specificatie | EtO Vergelijking |
|---|---|---|
| Cyclustijd | Minder dan 2 uur | 14+ uur |
| Infrastructuur | Alleen standaard vermogen | Processtoom, reductie |
| Facilitaire last | Lage kapitaalkosten | Hoge, gespecialiseerde ventilatie |
| Belangrijkste voordeel | Operationele efficiëntie | Microbiële penetratie |
| Inzet | Snel, flexibel | Complex, vast |
Bron: Technische documentatie en industriespecificaties.
Fase 3: Microbiologische validatie en naleving van ISO 22441
Wetenschappelijk bewijs verzamelen
In deze fase wordt theorie omgezet in bewezen steriliteitsgarantie. Het begint met het testen van de materiaalcompatibiliteit, waarbij monsters van hulpmiddelen worden onderworpen aan meerdere opeenvolgende VHP-cycli om te beoordelen op functionele of esthetische degradatie. Tegelijkertijd wordt microbiologische validatie per ISO 22441:2022 is verplicht. In het validatieplan moet een halfcyclische aanpak worden gebruikt om een reductie van minimaal 6 logs van geschikte biologische indicatoren aan te tonen. Geobacillus stearothermophilus sporen.
Worstcases valideren
De strategische nauwkeurigheid van validatie ligt in de reikwijdte ervan. Het moet rekening houden met worst-case belastingsconfiguraties en Process Challenge Devices (PCD's) gebruiken die de moeilijkst te steriliseren kenmerken vertegenwoordigen die in fase 1 zijn geïdentificeerd. Valideren onder geïdealiseerde omstandigheden is een kritieke fout; het proces moet op de proef worden gesteld met de maximale organische grondbelasting die bij routinematige verwerking wordt verwacht. Een parallelle vereiste is het valideren dat waterstofperoxideresten op apparaten en verpakkingen onder aanvaardbare limieten blijven, meestal 1-5 ppm.
Post-proces logistiek vereenvoudigen
Een belangrijk verschil met EtO is de weg na de sterilisatie. VHP valt uiteen in waterdamp en zuurstof, die definieert post-proces logistiek door de lange beluchtingstijden en complexe resttesten die nodig zijn voor EtO te elimineren. Dit vereenvoudigt de vrijgaveprocedures, verkort de verblijftijd in het magazijn en versnelt de productlevering aan de klant.
| Validatiecomponent | ISO 22441 Vereiste | Kritische parameter |
|---|---|---|
| Microbiële reductie | Minimaal 6-log reductie | Geobacillus stearothermophilus |
| Cyclusaanpak | Methode met halve cyclus | Aangetoonde dodelijkheid |
| Laadconfiguratie | Worst-case belasting | Process Challenge Devices (PCD's) |
| Resttests | limiet van 1-5 ppm | Waterstofperoxide concentratie |
| Stap na verwerking | Geen langdurige beluchting | Ontleedt tot water/zuurstof |
Bron: ISO 22441:2022 Sterilisatie van producten voor de gezondheidszorg - Verdampt waterstofperoxide bij lage temperatuur. Deze norm schrijft de vereisten voor VHP-procesvalidatie voor, inclusief de halfcyclische benadering, biologische indicatorselectie en worst-case belastingstesten om steriliteit te garanderen.
Fase 4: Protocollen voor operationele integratie en personeelstraining
Validatie omzetten in routine
Operationeel succes hangt af van de zorgvuldige integratie van het gevalideerde proces in de dagelijkse workflows. Ontwikkel apparaatspecifieke werkinstructies met betrekking tot voorbehandeling (indien nodig), goedgekeurde laadpatronen en selectie van cyclusparameters. Zorg voor een robuuste routinematige bewaking: fysieke parameters (tijd, temperatuur, concentratie) voor elke cyclus, chemische indicatoren voor elke lading en biologische indicatoren met een bepaalde frequentie per cyclus. ISO 14937:2009 principes.
Uitgebreide competentieontwikkeling
De training van het personeel moet verder gaan dan het indrukken van knoppen. Het moet gaan over de fundamentele technologieprincipes, veiligheidsprocedures voor het omgaan met geconcentreerd H₂O₂, alarmreactieprotocollen en het kwaliteitsbelang van elke stap. Een goed opgeleid team is essentieel om de snelle doorlooptijden te handhaven die de investering rechtvaardigen. De afhankelijkheid van nauwkeurige parametercontrole onderstreept waarom sensor- en gegevensanalyse worden cruciaal; Investeren in een geavanceerde bewakingsinfrastructuur is de sleutel tot het maximaliseren van de verwerkingscapaciteit en het behouden van de naleving van validaties.
Procesbetrouwbaarheid garanderen
De overgang van een gevalideerde toestand naar een toestand van routinematige controle vereist waakzaamheid. Implementeer een duidelijk proces voor afwijkingenbeheer en geef operators de bevoegdheid om de verwerking stop te zetten als kritieke parameters afwijken. Deze cultuuromslag naar gegevensgestuurd werken is net zo belangrijk als de technische installatie van de sterilisatieapparatuur met waterstofperoxide.
Fase 5: Updates van het kwaliteitssysteem en indiening bij de regelgevende instanties
De verandering formaliseren
De conversie moet formeel worden verankerd in uw kwaliteitsmanagementsysteem (QMS). Werk alle relevante documentatie bij: de kwaliteitshandleiding, samenvattende validatierapporten (IQ/OQ/PQ) en alle bijbehorende standaardwerkprocedures (SOP's). Implementeer een duidelijk wijzigingscontroleregister voor elke productfamilie die overgaat van EtO naar VHP en zorg voor volledige traceerbaarheid.
Het momentum van de regelgeving benutten
De regelgeving is nu gunstig voor het gebruik van VHP. De herclassificatie van VHP door de FDA in 2024 als “Established Category A” en de erkenning van ISO 22441 bieden een duidelijk, gestructureerd pad. Bereid wettelijke aanvragen voor (bijv. FDA 510(k) supplementen) om de sterilisatiemethode voor de betreffende hulpmiddelen bij te werken. Deze reguleringsmomentum proactief het nalevingsrisico op lange termijn vermindert in vergelijking met het handhaven van EtO-processen die steeds kritischer worden bekeken.
Communicatie met klanten beheren
Stel getroffen klanten proactief op de hoogte met een uitgebreid ondersteuningspakket. Dit omvat een formele validatieverklaring met een samenvatting van de aanpak en resultaten, en bijgewerkte sterilisatie-instructies voor hun basisregistraties. Transparante communicatie tijdens deze fase stelt het vertrouwen van de klant veilig en vermindert het commerciële risico.
Fase 6: Monitoring en optimalisatie na de implementatie
Key Performance Indicators vaststellen
Voor succes op de lange termijn is waakzaam toezicht nodig. Houd gedefinieerde KPI's bij, zoals non-conformiteitspercentages van cycli, positieve percentages van biologische indicatoren (doel: nul) en uptime/downtime van apparatuur. Door deze trends te analyseren, worden vroegtijdige tekenen van procesafwijkingen of slijtage van apparatuur opgespoord voordat ze van invloed zijn op de productkwaliteit.
Verplichte periodieke revalidatie
Houd je strikt aan het schema voor periodieke revalidatie zoals vereist door ISO 22441. Dit is niet optioneel; het is een vereiste om een staat van controle te behouden. Revalidatie moet worst-case belastingen opnieuw beoordelen, vooral als nieuwe apparaattypes worden geïntroduceerd in het VHP portfolio.
Een concurrerende marktpositie opbouwen
Zorg voor een formele feedbacklus met klanten om problemen met materiaalcompatibiliteit of functionaliteit op te sporen. Deze voortdurende optimalisatiecyclus is waar voordeel van de eerste stap in VHP-validatie wordt strategisch. De diepgaande, gepatenteerde proceskennis die is opgedaan bij het beheersen van VHP's parameters voor complexe apparaten creëert een aanzienlijke concurrentiemogelijkheid, waardoor de service zich beter onderscheidt.
| Essentiële prestatie-indicator (KPI) | Bewaking Doel | Strategisch resultaat |
|---|---|---|
| Cyclus Afwijkingen | Trendreductie | Procesbetrouwbaarheid |
| BI Positieve Tarieven | Nul positieven | Duurzame validatie |
| Stilstand van apparatuur | Minimaliseer | Doorvoer maximaliseren |
| Periodieke revalidatie | ISO 22441 schema | Continue naleving |
| Feedbacklus voor klanten | Detectie van problemen | Concurrerende kennis slotgracht |
Bron: ISO 22441:2022 Sterilisatie van producten voor de gezondheidszorg - Verdampt waterstofperoxide bij lage temperatuur. De standaard beschrijft de eisen voor routinematige controle en monitoring, inclusief de frequentie van biologische indicatortesten en de noodzaak voor periodieke revalidatie om een staat van controle te behouden.
Belangrijke beslissingsfactoren voor uw VHP conversie tijdlijn
Interne drijfveren: Portfolio en middelen
Uw tijdlijn wordt in de eerste plaats bepaald door interne factoren. De complexiteit van uw hulpmiddelenportefeuille uit Fase 1 is van het grootste belang; een portefeuille met veel complexe, op lumen gebaseerde hulpmiddelen zal een langere, uitgebreidere validatiecyclus vereisen dan een portefeuille met eenvoudige oppervlaktehulpmiddelen. Intern zal de beschikbaarheid van gekwalificeerd personeel voor het uitvoeren van validatiestudies en het geven van training direct invloed hebben op uw voortgang.
Externe afhankelijkheden: Regelgeving en apparatuur
Externe factoren zorgen voor variabele tijdlijnen. Regelgevende indieningsstrategieën voor elke hulpmiddelenfamilie kunnen onvoorspelbare beoordelingsperioden met zich meebrengen. Hoewel de doorlooptijd voor de aanschaf en installatie van VHP-apparatuur over het algemeen korter is dan voor EtO vanwege de lagere infrastructuureisen, moet er toch rekening mee worden gehouden in het kritieke pad. Het is van cruciaal belang dat u de opkomend servicemodel voor niche EtO; als er enige EtO-capaciteit wordt behouden, is het voor de algehele bedrijfscontinuïteit noodzakelijk om te plannen voor de mogelijke consolidatie ervan en de hogere prijzen.
| Beslissingsfactor | Impact op tijdlijn | Voorbeeld Variabele |
|---|---|---|
| Complexiteit apparaat | Hoog (Fase 1-audit) | Materiaal/geometrisch toepassingsgebied |
| Strategie voor regelgeving | Variabele herzieningsperioden | FDA 510(k) supplementen |
| Interne bronnen | Stappen validatie/training | Beschikbaarheid personeel |
| Doorlooptijd apparatuur | Over het algemeen korter dan EtO | Inkoop en installatie |
| EtO servicemodel | Bedrijfscontinuïteitsplanning | Behoud van nichecapaciteit |
Bron: Technische documentatie en industriespecificaties.
Een aangepaste conversieroutekaart en offerte aanvragen
Een algemene checklist geeft richting, maar voor de uitvoering is een plan nodig dat is afgestemd op uw unieke hulpmiddelenportfolio, de beperkingen van de faciliteit en de commerciële doelstellingen. Een gedetailleerde routekaart vat de bovenstaande fasen samen in een projectplan met specifieke mijlpalen, toewijzing van middelen en strategieën voor risicobeperking. Het biedt een realistisch tijdschema en investeringsprofiel, waardoor een weloverwogen kapitaalplanning mogelijk is.
De overgang van ethyleenoxide naar VHP-sterilisatie is een technische en strategische onderneming in meerdere fasen. Het succes hangt af van een eerlijke portfolio-audit, een validatie die is verankerd aan ISO 22441 en een operationele integratie die de doorvoervoordelen van VHP benut. De beslissing om door te gaan vereist een evenwicht tussen de wettelijke vereisten en de technische haalbaarheid van uw specifieke mix van hulpmiddelen.
Behoefte aan een professionele beoordeling en een implementatieplan op maat voor uw sterilisatieomschakeling? De experts van QUALIA kan een gedetailleerde audit en een stappenplan leveren op basis van uw specifieke portfolio en operationele doelen. Neem contact met ons op om je vereisten te bespreken en een haalbaarheidsonderzoek te plannen.
Veelgestelde vragen
V: Hoe bepalen we welke hulpmiddelen in onze portfolio geschikt zijn voor de conversie van EtO- naar VHP-sterilisatie?
A: Voer een gedetailleerde controle uit van elk hulpmiddel en documenteer de materialen, geometrie, verpakking en geschiedenis van de biobelasting. Deze gegevens wijzen op hulpmiddelen met bekende VHP-beperkingen, zoals oxidatiegevoelige polymeren, ongecoat koper of lange, smalle lumina met een diameter van minder dan 1 mm. Het strategische resultaat is een duidelijke splitsing tussen VHPcompatibele apparaten en apparaten die EtO moeten blijven gebruiken. Verwacht voor projecten met complexe portefeuilles aanzienlijke middelen voor deze technische screening en mogelijke materiaalherontwerpen met leveranciers.
V: Wat zijn de belangrijkste verschillen in de infrastructuur van een faciliteit bij de overstap van een EtO- naar een VHP-systeem?
A: VHP-systemen hebben meestal alleen standaard elektrische voeding nodig, waardoor processtoom, reductie van gevaarlijke gassen en gespecialiseerde ventilatie die vereist is voor ethyleenoxide niet nodig zijn. Dit vermindert drastisch de infrastructuurlast van de faciliteit en de bijbehorende kapitaalkosten. Het operationele voordeel is aanzienlijk en maakt een snellere en flexibelere inzet in bestaande ruimtes mogelijk. Dit betekent dat faciliteiten met ruimte- of utiliteitsbeperkingen de voorkeur zouden moeten geven aan VHP vanwege de lagere complexiteit van de installatie en de snellere operationele opstart.
V: Wat is de vereiste microbiologische validatiebenadering voor een nieuw sterilisatieproces voor VHP's?
A: Validatie moet volgens de halfcyclische methode per ISO 22441 om een minimale reductie van 6 log van resistente biologische indicatoren aan te tonen. Het plan moet worst-case belastingsconfiguraties en Process Challenge Devices (PCD's) testen die uw moeilijkst te steriliseren apparaatkenmerken vertegenwoordigen. Deze basisvereiste van ISO 14937 betekent dat de reikwijdte en duur van je validatie direct worden bepaald door de complexiteit van je portfolio, dus plan uitgebreide tests voor apparaten met uitdagende geometrieën of materialen.
V: Hoe verandert de behandeling na sterilisatie bij de overgang van EtO naar VHP?
A: VHP ontbindt in water en zuurstof, waardoor de langdurige beluchtingscycli en complexe resttesten die nodig zijn voor ethyleenoxideresiduen komen te vervallen. Dit vereenvoudigt de logistiek na het proces, vermindert de voorraad onderhanden werk en versnelt de productvrijgave. Als uw bedrijf een snelle doorlooptijd en een hoge flexibiliteit in de toeleveringsketen vereist, bieden de kortere cyclustijden en het ontbreken van beluchting van VHP een duidelijk operationeel voordeel ten opzichte van traditionele EtO-processen.
V: Wat zijn de kritieke factoren die de tijdlijn bepalen voor een volledig EtO naar VHP conversieproject?
A: Uw tijdlijn is afhankelijk van de complexiteit van de productportefeuille, de strategie voor het indienen van aanvragen bij de regelgevende instanties voor elke productfamilie, de beschikbaarheid van interne middelen voor validatie en de doorlooptijd van de apparatuur. De omvang en duur van de vereiste ISO 22441 Validatiestudies zijn de meest variabele factor. Dit betekent dat faciliteiten met veel complexe, op lumen gebaseerde apparaten rekening moeten houden met een langere tijdlijn in meerdere fasen, terwijl faciliteiten met eenvoudigere portfolio's sneller kunnen omschakelen.
V: Waarom is training van het personeel bijzonder belangrijk voor een betrouwbare werking van VHP in vergelijking met EtO?
A: De effectiviteit van VHP hangt af van een nauwkeurige controle van kritieke parameters zoals dampconcentratie, vochtigheid en temperatuur tijdens de cyclus. Uitgebreide training moet de technologische principes, het omgaan met geconcentreerde waterstofperoxide en specifieke alarmreactieprotocollen omvatten. Deze operationele afhankelijkheid van nauwkeurige parametercontrole betekent dat investeren in geavanceerde sensorbewaking en gegevensanalyse essentieel is voor het handhaven van de validatieregelgeving en het maximaliseren van de verwerkingscapaciteit in omgevingen met grote volumes.
V: Hoe moeten we onze regelgevingsstrategie aanpassen als we een verandering van EtO- naar VHP-sterilisatie indienen?
A: Werk de documentatie van uw kwaliteitsmanagementsysteem bij, inclusief validatierapporten en SOP's, met een duidelijke wijzigingscontrole. De herclassificatie in 2024 van VHP's door de FDA als “Established Category A” en de erkenning van ISO 22441 zorgen voor een gunstig regelgevend pad. Bereid aanvragen voor zoals 510(k) supplementen om de sterilisatiemethode bij te werken. Dit momentum in de regelgeving betekent dat u gebruik moet maken van de huidige duidelijkheid om het nalevingsrisico op de lange termijn te verminderen en uw commerciële licentie voor de nieuwe service veilig te stellen.
Gerelateerde inhoud:
- Sterilisatie met verdampte waterstofperoxide vs. ethyleenoxide: 8 cruciale verschillen voor fabrikanten van medische hulpmiddelen
- Vereisten voor materiaalcompatibiliteitstesten voor VHP sterilisatie: ISO 22441 protocolgids
- VHP vs. Traditionele Sterilisatie: 2025 Vergelijking
- VHP Sterilisatie in de gezondheidszorg: 2025 Beste Praktijken
- GMP VHP Generatoren | FDA Vereisten voor Draagbare Ontsmetting
- De Complete Waterstofperoxide Sterilisatiegids voor Medische Apparaten en Farmaceutische Instellingen: 2025 Standaarden en Beste Praktijken
- VHP sterilisatieproces: 2025 Uitgebreide Gids
- Top 10 voordelen van VHP sterilisatie in 2025
- Laboratoriumsterilisatie met VHP: 2025 gids voor experts